

Tuesday 19 February 2019,
by Andy Stafford
I joined my colleague Peter Mortimore at ‘Empowering people in a digital world’ run by and primarily for the NHS, in London 13th February 2019. Whilst as a business nitro works internationally, I am British and have more than a passing interest in how the NHS is leveraging or dealing with, the promise and challenge of technology to deliver new models of care, efficiencies and improved health outcomes for patients. Because, along with family and friends, I will, of course, be the beneficiary of that care.
The NHS is a massive employer (1M+) and a highly complex beast, that I imagined, in spite of the undoubted talent at its disposal, would still be making heavy work of the digital opportunity. However, what we heard from Matthew Swindells and Tara Donnelly was real ambition, supported by a focused and coherent plan that seemed to make real sense. The vision is in three parts which included staying healthy and preventing illness, intuitive self-service, and personalisation. It aligns perfectly with our purpose to ‘bridge the gap to healthier lives’ by delivering health outcomes through, (primarily) digital innovation, whether with life science, experts, patients, or the providers like the NHS or by collaborating with everyone simultaneously.
Government and senior leadership in the NHS are universally ‘excited’ about digital (okay, better late than never I suppose!), and committed to ensuring that it is incrementally rolled out and adopted in an agile manner (rather than all at once has been the aim in previous initiatives) whilst taking care not to exclude those without access or appetite for digital, which of course is a dwindling, but still significant number.
So, what is the NHS doing?
Matt Hancock, the Secretary of State for Health and Social Care, presented a practical internal view of upcoming changes, citing that email, rather than mail or even fax, as being the standard operating procedure by which internal and external to patient communication will be conducted. It seems that the privacy fears are largely discounted in favour of speed, efficiency and patient health, which seems sensible. There is an estimated £8m a year spent on paper, £2m in envelopes, and the NHS remains the biggest purchaser of fax machines in the world. As he pointed out, and I’ll paraphrase, ‘we’ve conducted a test to see if people will use email and it turns out 4BN people are happy to do so’. It’s time to join modernity.
It is said that ‘language is the most powerful tool of a revolution’ so it was really reassuring to hear the NHS using words and phrases throughout the day from Polly Bishop, Michael Ekpe and Tara Donnelly through to Matt Edgar & Caroline Jarrett like, ‘predictive prevention’, ‘agile’, ‘user-centered design’, to ideas like focusing on the specific person and designing for the variances, focussing on cause not prevention, and build test, measure, learn, and adapt. You got the distinct feeling that they were not just being used as buzzwords but fundamental to how the NHS is approaching digital transformation.
To make digital meaningful and integral to patients the NHS is starting with three key elements. First, a revamped NHS website (previously known as ‘NHS choices’), and a patient app (who knew!?) within a fully interoperable ecosystem that includes patient records (PHR) into which the best of industry ideas and offerings in terms of tech, content, and services can be incorporated. The NHS app already has 800,000 downloads and is complemented by the colossal NHS website at the beating heart of the planned ecosystem with 40,000+ content pages that are being designed and rolled out with and around users.
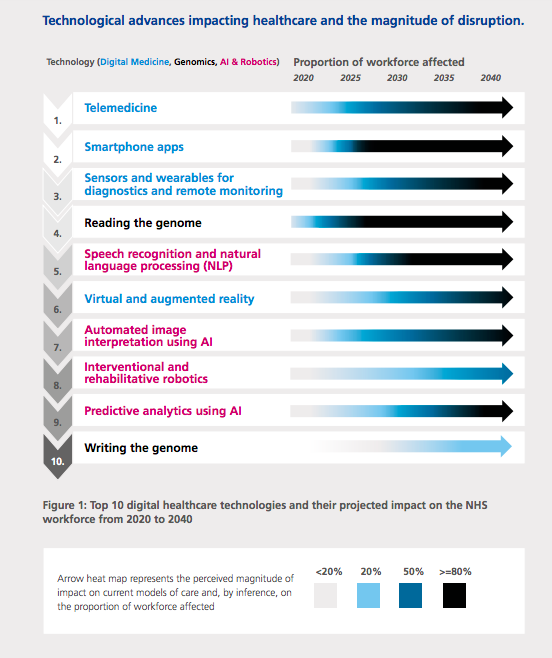
Earlier in the week, Dr. Topol released his Topol report outlining how healthcare workers can prepare to deliver for the digital future. He identified the importance and impact of certain technologies in the healthcare system of the future, and the crucial point that the NHS accepts that it cannot do everything and instead that it must work collaboratively to encourage and foster ideas, develop initiatives and solutions that integrate into their ecosystem and app offering. Through intermediaries like the health accelerators ‘AHSN’s’ and ‘Innovate UK’ it is anticipated they will be able to solve more problems, more quickly, for the NHS and the patients being served.
Top 10 digital healthcare technologies and their projected impact on the NHS workforce from 2020 to 2040
There is a roadmap for PHR or ‘Personal Health Records’, known more generally as EHR. I first heard the NHS planning to deliver our records back in the early 2000s in a, quite obviously an unsuccessful (but lavishly budgeted) project and had consequently filed the idea of UK patients getting access to their health records firmly into the category of sci-fi. Happily, it seems I am wrong. There is a five-step process to making individual healthcare records useful and available across the continuum of care to healthcare professionals and the individual themselves within a fully interoperable two-way system. In fact, some trusts within the UK are already achieving progress and a toolkit to aid learning and adoption.
PHR is live within 11 NHS trusts and being used by 22 speciality units in Southampton. Piloted within ‘Southampton University Hospital’ a new model of care case study for prostate cancer was shared that demonstrated that a significant increase in the number of patients that could be processed effectively. When the patients shared their tracking data with the care team the number that could be processed increased from six, that would be seen face to face in the clinic, to up to thirty online. By providing their PSA readings patients could be dealt with more efficiently, at greater convenience to them, whilst also allowing for greater care to be provided to those that actually needed it, in a more timely manner than their three-monthly routine appointment would ever allow.
A great deal of effort is being placed into governance and standards too. Of course, there won’t be a randomised, double-blind, placebo run clinical trial involving one thousand subjects for apps and other digital interventions though. It’s not practical, as Dr Indra Joshi explained. The nature of apps and other digital services, unlike rigorously produced pharmaceutical medicines, is that they will evolve to enhance their utility, and necessarily on a continual basis.
A collaborative future
That does not mean that the app’s efficacy, the producer, the experience of its users, and cost-effectiveness cannot be judged though. And perhaps this presents an opportunity for life science companies? Why not include digital service as one arm of the clinical trial in order to understand if the digital component not only improves patient outcomes but can be designed in such a way that it reduces the burden on the health service in which it is provided? Well designed, the digital component could offer, for instance, critical data and practical and behavioural support to keep patients motivated and collaborating with their care team. This makes the solution compelling for patients, professionals, and the payer.
Non-adherence is, of course, a massive issue, with dire consequences including poorer patient outcomes such as unsatisfactory quality of life, increased hospitalisations, shorter life and even death (Medication non-adherence: what can the pharmaceutical industry do to prevent this “silent killer”?). But also negatively impacts the systems providing the care and their ability to provide the care needed by everyone. Digital support and interventions should be designed from the outset.
There is an opportunity for big pharma, in particular, as they have as much incentive to deliver real patient outcomes as public health systems do, and much greater resources to accomplish this aim with. They must look into how they can expand their product offering to extend support to the ‘whole human’ to help national health providers globally deliver care cost-effectively as the costs continually look set to increase.
Tackling the obvious ‘big’ challenges like obesity (which is linked to cancers, heart and liver disease, for instance) and dementia which are only going to get bigger is a great place to start. These and other disease areas offer enormous opportunities for industry to provide real value to all stakeholders. 30,000 elderly patients are to be found in specialist hospital care ward beds every day that don’t actually need them. This is a complex problem, but technology such as health tracking, remote-care, AI, VR, and all the rest will contribute to a solution that simultaneously keeps the elderly out of a hospital, living fuller connected lives (addressing this goes well beyond treating a disease) and reduces the burden on the health system.
Meaningful solutions, however, require insight and co-creation through a relationship with the patients that are developed much earlier and more deeply and improved iteratively based on data and feedback (i.e. agile, and GDD for instance) that is the case for pharma right now. As is argued in a previous paper this closer relationship would be welcomed by patients.
Someone mentioned that the NHS needed to be just that, ‘national health’ rather than ‘national sickness’. Whilst sounding like a pithy soundbite, it is a critical point that requires a shift in mentality from curing to preventing. An explicit shift not only to more preventative medicine but also to greater personal responsibility. Until genomic testing, and A.I., for instance, become advanced and universal it will still be beholden on the individual to contribute to their own health and in doing so help make the system work for everyone.
Whilst the U.K. does not provide a perfect template for other national health care providers the logic behind user-focused digital support and intervention will be reapplied elsewhere in Europe and the world. Further, user-focused solutions that are agile and never finished that should be delivered collaboratively and never done are themes that are universal. Fresh insightful ideas need to be tested and integrated into an open ecosystem to improve health and wellness for everyone.

